I wrote in our September newsletter about how trial sponsors are well advised to view transparency as much more than just a box that has to be checked off. This time, I would like to dig deeper into how sponsors can bring new life to their data and drive innovation across the entire drug development lifecycle.
The health care industry is rapidly evolving. Drug companies are being called upon to embrace an operating model that is anchored by collaboration, openness and trust. Those of us in the transparency space have seen a continued shift in the landscape, with greater expectation for clinical trial transparency and data sharing. Regulatory shifts are of course reflecting this expectation.
This has required drug companies to develop transparency capabilities, such as anonymization, to ensure data can be shared in a privacy-preserving manner, efficiently and at scale, without losing the utility, or secondary research value, of the data.
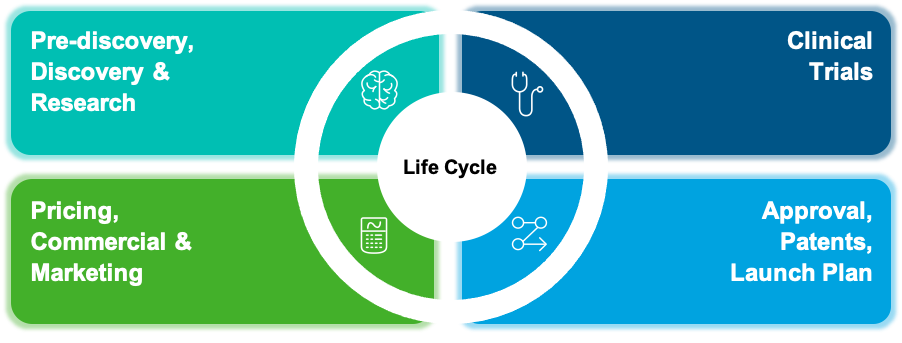
Once organizations establish the necessary anonymization processes to drive clinical trial transparency (CTT), this same capability can be leveraged further along the drug development life cycle.
Let’s examine this across the four major stages of that life cycle.
Stage 1: Pre-discovery, Discovery, Research
Here, large volumes of clinical trial, DICOM and real-world data can be pooled into data lakes and data platforms to accelerate internal innovation.
We have seen examples where trial sponsors have leveraged the anonymization capabilities developed to achieve transparency, to make data more accessible and re-usable internally. This has fueled innovation and drug discovery, the evaluation of new hypotheses, and extended scientific discoveries beyond those derivable from any single trial or dataset.
Stage 2: Clinical Trials
At this stage, sponsors can maximize the efficiency and throughput of trial data sharing with other external researchers for transparency. This is important to meet the rising expectations for more open data sharing across the research ecosystem.
As I wrote last time, transparency can also influence reputation and trust in a brand. These factors will impact outcomes such as patient recruitment for trials. The right anonymization approach can help achieve transparency while also ensuring the privacy of trial participants, which are both critically important to build trust.
Stage 3: Approvals, Patents, Launch Plan
Regulatory deadlines are the chief concern here – meeting the European Medicines Agency’s Policy 0070, Health Canada’s Public Release of Clinical Information (PRCI) or other regulatory deadlines for anonymized clinical study documents. These policies require that clinical study documents be anonymized and published, and the deadlines can be tight.
Both the EMA and Health Canada endorse a risk-based and quantitative anonymization approach that is consistent with other emerging standards for anonymization around the world. This growing trend is in sharp contrast to the traditional redaction methods that were favoured up to relatively recently.
What is the difference between a risk-based and quantitative anonymization approach versus traditional redaction? It’s all about removing what’s identifiable in the data while preserving what’s useful or valuable. In our previous newsletter, I offered the example of a 34-year-old female patient with Coeliac disease.
In all instances, the key is that the risk of re-identification of any one patient or trial participant be reduced below a threshold that is acceptable to the regulator. For transparency purposes, this must be achieved in a manner that preserves the utility of the data (i.e. minimizes the information loss).
Stage 4: Pricing, Commercial & Marketing
Which brings us to the last phase of that life cycle – differentiation. When real-world data can be safely sourced and linked, it can illuminate the actual impact that a drug treatment has on the lives of patients. This enables commercialization and market access.
For example, we had one client that wanted to study the clinical effectiveness of a metabolic syndrome drug a couple of years into the market. With data sourced from health clinics that prescribed the drug, we employed statistical anonymization to preserve all the utility required by researchers, while ensuring that nothing personally identifying remained in the data. The result was a published study of real-world evidence of drug efficacy with clinically meaningful weight loss results.
In conclusion
Drug companies/trial sponsors have an opportunity to go beyond transparency and lever some of that same capability for greater benefit.
We often see a progression where the starting point can be meeting regulatory requirements, to then voluntarily sharing documents or structured patient data with researchers to further promote transparency, and then going even further by using the same methodology and statistical techniques to support a wide range of internal data sharing and re-use scenarios that may include linking with real-world data.
The result is the full value of the data is harnessed while ensuring privacy – and ultimately, brand trust.
This article is drawn from a recent webinar that I presented for the CBI’s 9th Annual Publications and Clinical Trial Transparency conference in September. You can view a recording of this session here on our website.